So you’re considering dental implants and wondering about the success rate and if they’re a good solution for your missing teeth.
With concerns about dental implant failure, cost and overall health, you need to know what affects their success.
What is the Success Rate of Dental Implants?
The success rate of dental implants is approximately 95–98% over a 5-year period, with factors such as implant length, diameter, and patient health influencing outcomes. According to recent studies, implants with lengths over 10 mm and diameters over 3.75 mm have higher survival rates, with 5-year survival rates of 94.5% and 96.2%, respectively.
| Factor | Description | Impact on Success Rate |
|---|---|---|
| Implant Length and Diameter | Longer and wider implants generally provide better stability and integration. | Implants >10 mm and >3.75 mm have survival rates of 94.5% and 96.2% respectively (10). |
| Patient Health | Overall health, including management of chronic conditions, affects healing and integration. | Proper management of conditions like diabetes can enhance success rates (6). |
| Surgical Technique | Precision in placement reduces complications and improves outcomes. | Experienced surgeons have higher success rates (9). |
| Aftercare | Regular check-ups and good oral hygiene prevent complications. | Improves implant longevity and reduces failure risk (8). |
Factors that Affect the Success Rate of Dental Implants
Age and Health of the Patient
Age and overall health of the patient are big factor in the success of dental implants.
Younger patients have better bone quality, which makes osseointegration easier—the process where the implant integrates with the jawbone.
But older patients can still achieve high success rates if they take good care of their oral health and manage their chronic conditions well (4).
Bone Quality: Good bone is essential for implant stability and longevity.
Patients with osteoporosis or other bone-related conditions may have challenges but advancements in implant technology and surgical techniques can minimize the risks (4).
Chronic Conditions: Diabetes and cardiovascular diseases can affect healing and increase the risk of complications.
Proper management and pre-surgical assessments are key to minimizing these risks (6).

Type of Implant
The type and quality of the dental implant affect the success rate.
Implants made from high-quality materials like titanium are known for their durability and biocompatibility (1).
Material: Titanium is the material of choice because it bonds well with bone and is corrosion-resistant.
Surface modifications like roughening enhances osseointegration and stability (4).
Design: The design of the implant, length and diameter, affects the success.
Longer and wider implants have higher survival rates: a 5-year survival rate of 94.5% for implants over 10 mm and 96.2% for implants over 3.75 mm (10).

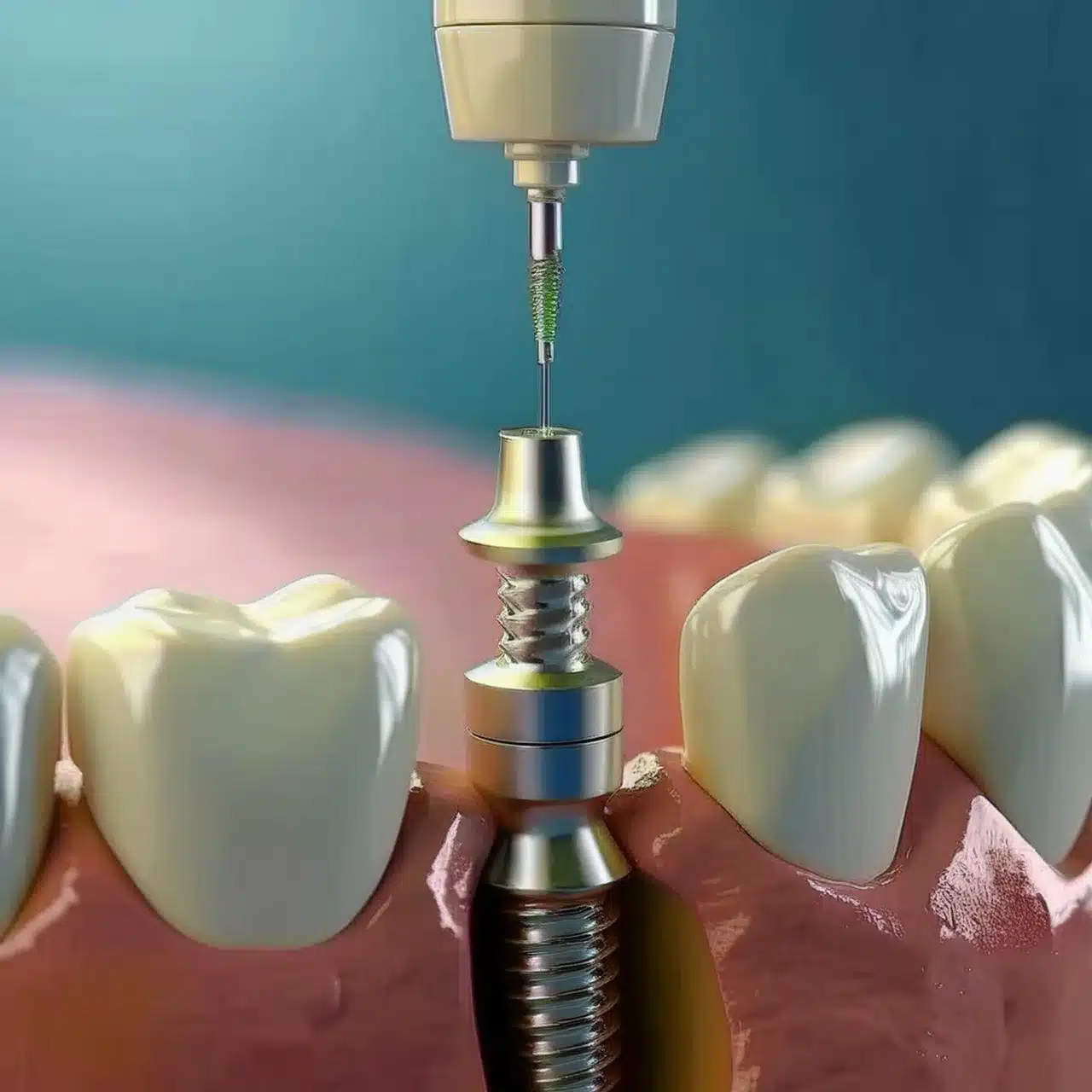
Dental Implant Surgery Technique and Surgeon’s Experience
The surgeon and the surgical technique used are big factors in the success of dental implants.
Skilled surgeons can minimize trauma to the bone and surrounding tissues and reduce the risk of complications (9).
Surgical Precision: Precise placement of the implant is crucial to avoid damage to nerves and blood vessels.
Advanced imaging and computer-guided surgery have improved placement accuracy (8).
Experience: Surgeons with more experience in implantology have higher success rates because they can anticipate and manage potential complications (9).
| Factor | Description | Impact on Success Rate |
|---|---|---|
| Implant Length and Diameter | Longer and wider implants generally provide better stability and integration. | Implants >10 mm and >3.75 mm have survival rates of 94.5% and 96.2% respectively (10). |
| Patient Health | Overall health, including management of chronic conditions, affects healing and integration. | Proper management of conditions like diabetes can enhance success rates (6). |
| Surgical Technique | Precision in placement reduces complications and improves outcomes. | Experienced surgeons have higher success rates (9). |
| Aftercare | Regular check-ups and good oral hygiene prevent complications. | Improves implant longevity and reduces failure risk (8). |
Dental Implant Longevity
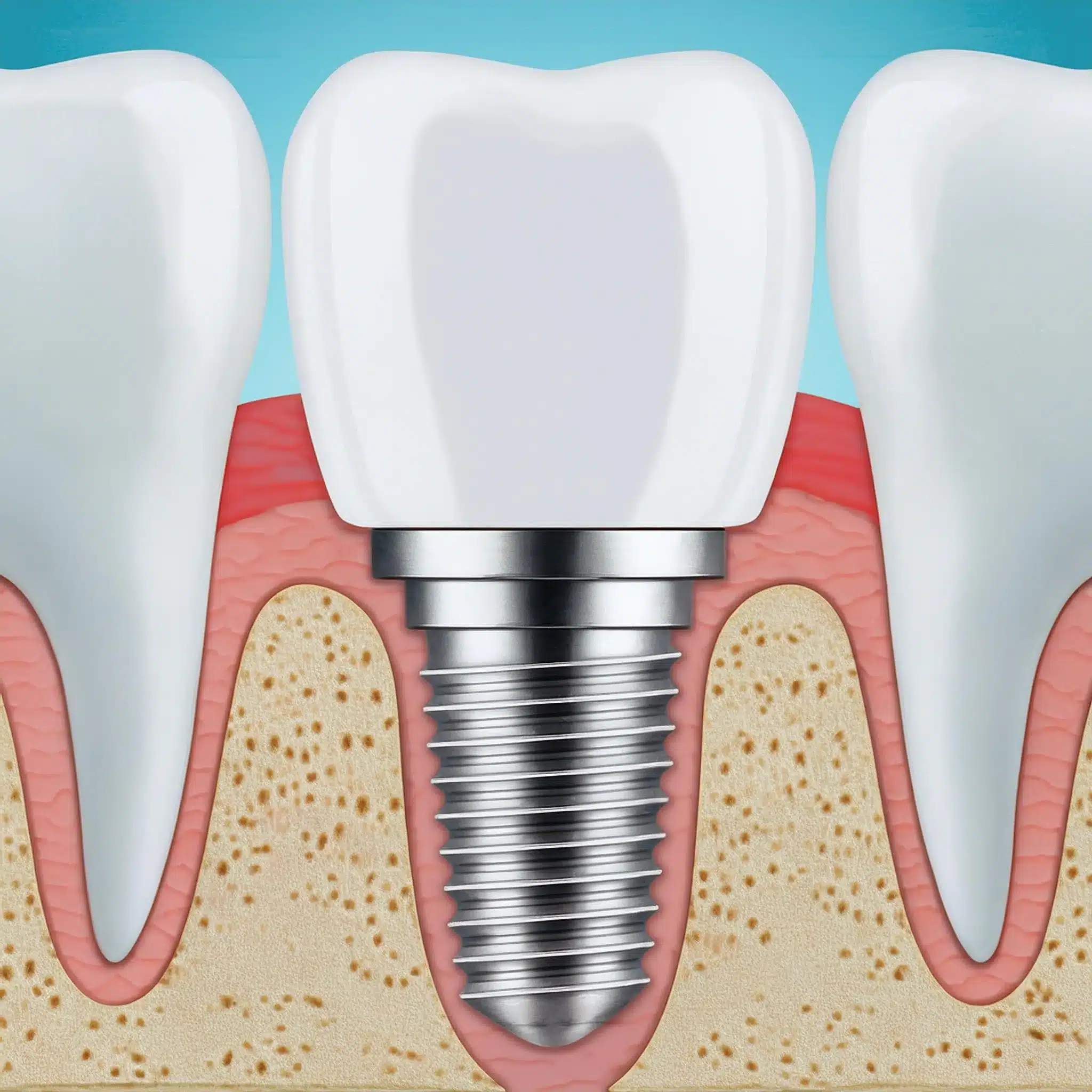
Osseointegration and Its Significance
Osseointegration is the biological process where the implant fuses with the jawbone to form a stable and long-lasting bond.
This process is key to long-term success and stability of dental implants (2).
Bone Integration: The implant surface interacts with the bone, osteoblasts deposit bone matrix and the bond gets stronger over time (3).
Material: Titanium’s biocompatibility promotes osseointegration, and surface modifications enhance this integration and lead to better implant stability (5).
Clinical Outcomes: High degree of osseointegration correlates to lower failure rates; studies show above 90% success rate for well integrated implants (7).
Dental implants offer numerous benefits and advantages, including the ability to mimic natural tooth function and aesthetics, prevent bone loss, and provide a long-lasting solution compared to other options.
Many people, including celebrities with dental implants, have chosen this option to enhance their smiles and oral health.
When issues arise, dental implant repair becomes necessary to address complications and restore the function and appearance of the implants.
This process may involve replacing damaged components, treating infections, or adjusting the implant position to ensure stability and longevity.

Effect of Proper Aftercare on Longevity
Proper aftercare is key to maintaining dental implant longevity.
It means regular dental check-ups and good oral hygiene practices to prevent complications like peri-implantitis (8).
Oral Hygiene: Brushing and flossing regularly is crucial to prevent infection and inflammation around the implant site (8).
Professional Monitoring: Regular dental visits helps monitor the health of the implant and surrounding tissues and detect potential issues early (8).
Lifestyle: Avoiding smoking and managing chronic conditions like diabetes can significantly enhance implant longevity by promoting better healing and integration (6).
Comparative Analysis of Different Implant Types
Endosteal vs. Subperiosteal Implants
Dental implants come in different types; endosteal and subperiosteal are two of the most common.
Understanding the difference between these two is crucial in choosing the right one based on individual needs and anatomical consideration (3).
Endosteal Implants: This is the most common type of dental implant.
Made from biocompatible materials like titanium, it is surgically placed into the jawbone.
This type of implant has excellent stability and is suitable for patients with adequate bone density.
However, it requires a surgical procedure and longer healing time (4).
Subperiosteal Implants: This implant is placed on top of the jawbone but beneath the gum tissue.
It is ideal for patients with insufficient bone density who want to avoid bone grafting.
Less invasive, subperiosteal implants may not have the same long-term stability as endosteal implants (5).

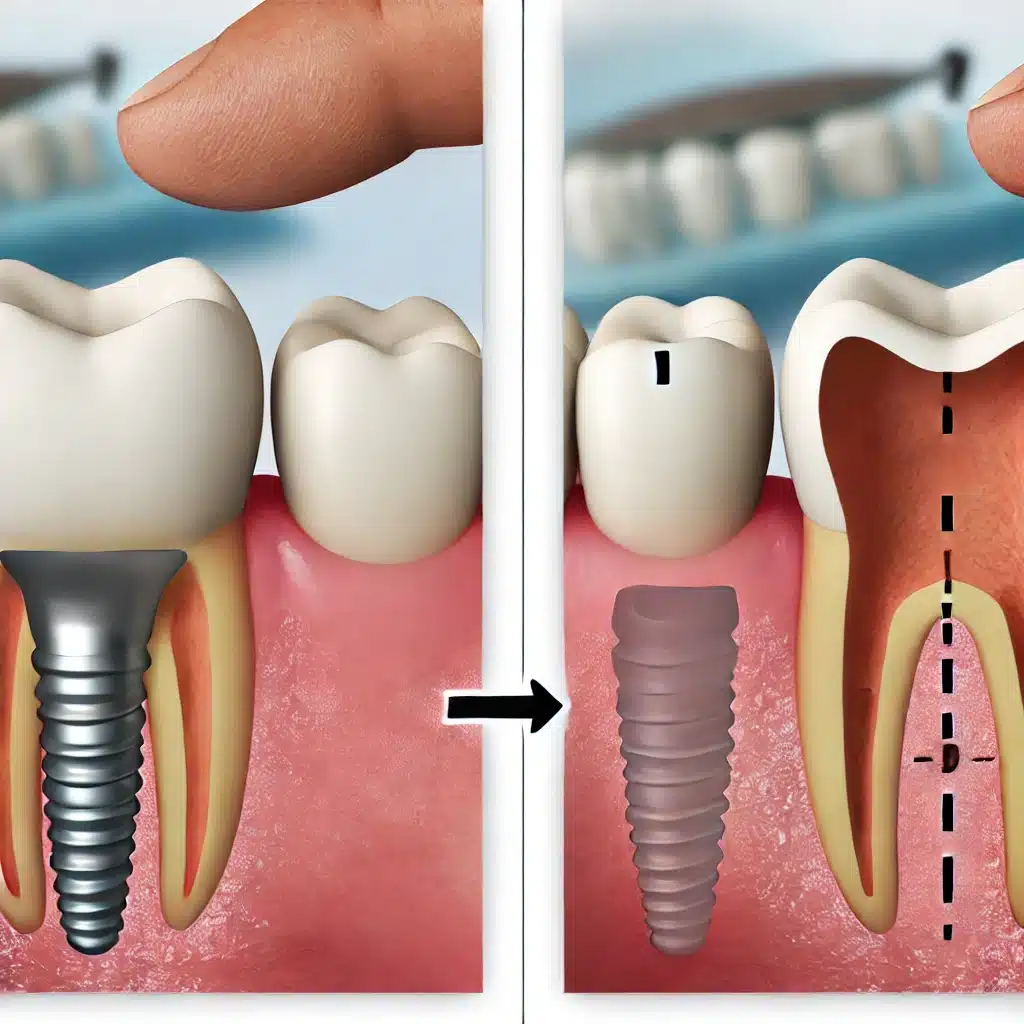
Immediate vs. Delayed Implant Placement
The timing of implant placement can impact the outcome and success rate of dental implants.
Immediate and delayed placement each have their own advantages and considerations (2).
Immediate Implants: Placed at the same time as tooth extraction, they reduce the number of surgical procedures and overall treatment time.
Immediate implants can preserve bone and soft tissue architecture and offer aesthetic benefits.
However, it requires precise surgical technique and is not suitable for all patients (2).
Delayed Implants: This approach involves placing the implant after the extraction site has healed, usually 3-6 months.
Delayed placement allows for better assessment of the bone and tissue condition and a potentially higher success rate in complex cases.
However, it requires longer treatment time and additional surgical procedures (2).
Conclusion & Key-Takeaways
Key Takeaways:
Dental implants have a high success rate of 95-98% for over 5 years.
Implant length, diameter, patient health, and surgical technique affect the success rate of dental implants.
Proper aftercare is key to implant longevity.
Conclusion:
Dental implants are a reliable tooth replacement solution with a high success rate when managed properly.
By knowing the factors that affect its success and following aftercare guidelines, patients can have long-lasting and functional dental implants.

FAQ
References
(1) Albrektsson T, Zarb G, Worthington P, et al. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1(1):11-25.
Article: The long-term efficacy of currently used dental implants: a review and proposed criteria of success
(2) Pjetursson BE, Thoma D, Jung R, et al. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implants Res. 2012;23 Suppl 6:22-38.
(3) Jung RE, Zembic A, Pjetursson BE, et al. Systematic review of the survival rate and incidence of biologic, technical, and esthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin Oral Implants Res. 2012;23 Suppl 6:2-21.
(4) Buser D, Sennerby L, De Bruyn H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends, and open questions. Periodontol 2000. 2017;73(1):7-21.
(5) Esposito M, Grusovin MG, Coulthard P, et al. The efficacy of various bone augmentation procedures for dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants. 2006;21(5):696-710.
(6) Chrcanovic BR, Albrektsson T, Wennerberg A. Dental implants inserted in male versus female patients: a systematic review and meta-analysis. J Oral Rehabil. 2015;42(9):709-722.
Article: Dental implants inserted in male versus female patients: a systematic review and meta-analysis
(7) Klinge B, Meyle J. Soft-tissue integration of implants. Consensus Report of Working Group 2. Clin Oral Implants Res. 2006;17 Suppl 2:93-96.
Article: Soft-tissue integration of implants. Consensus Report of Working Group 2
(8) Papaspyridakos P, Chen CJ, Chuang SK, et al. A systematic review of biologic and technical complications with fixed implant rehabilitations for edentulous patients. Int J Oral Maxillofac Implants. 2012;27(1):102-110.
(9) Misch CE, Perel ML, Wang HL, et al. Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 2008;17(1):5-15.
(10) Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res. 2006;17 Suppl 2:35-51.
Article: Impact of implant length and diameter on survival rates