Shartimi i kockave është një pjesë e madhe e shumë procedurave dentare dhe ortopedike, por cilat janë rreziqet dhe përfitimet dhe si e zgjidhni transplantin e duhur për ju?
Nëse po konsideroni implantet dentare ose keni defekte të kockave, duhet të kuptoni shartimin e kockave për të marrë vendime të informuara për shëndetin tuaj.
Çfarë është shartimi i kockave?
Shartimi i kockave është një procedurë kirurgjikale që përdoret për të riparuar kockat përmes transplantimit të indit kockor, thelbësor për implantet dentare dhe trajtimin e defekteve të kockave. Së bashku me shartimi i indeve, përfaqëson një përparim thelbësor në mjekësinë rigjeneruese. Llojet kryesore përfshijnë graftet autograft, alograft, ksenograft, sintetikë dhe aloplastikë.

Llojet e Grafteve të Kockave
Autotransformim
Autograftet janë standardi i artë në shartimin e kockave për shkak të shkallës së lartë të suksesit dhe përputhshmërisë së tyre.
Ato përfshijnë mbledhjen e kockave nga trupi i vetë pacientit, zakonisht nga ijë ose nofulla.
Kjo zvogëlon rrezikun e refuzimit dhe përshpejton procesin e shërimit pasi ka qeliza të gjalla.
Pro:
Shkalla e lartë e suksesit për shkak të përputhshmërisë biologjike.
Nuk ka rrezik të transmetimit të sëmundjes.
Integrim dhe shërim më të shpejtë.
Kundër:
Kërkon një vend të dytë kirurgjik, i cili mund të rrisë kohën e rikuperimit dhe shqetësimin.

Alograft
Alograftet përdorin kockë nga një dhurues, e cila përpunohet për siguri dhe sterilitet.
Këto grafte janë lehtësisht të disponueshme dhe nuk ka nevojë për një operacion të dytë për të korrur kockën.
Pro:
Nuk ka nevojë për kirurgji shtesë për të korrur kockën.
E disponueshme në forma të ndryshme (pluhur, patate të skuqura, blloqe) për t'iu përshtatur nevojave të ndryshme.
Kundër:
Rrezik i vogël i transmetimit të sëmundjes (shumë i ulët për shkak të përpunimit).
Integrim më i ngadalshëm në krahasim me autotransplantet.
Ksenograft
Ksenograftet janë nga burime jo njerëzore, zakonisht nga gjedhi.
Ato përpunohen për të hequr të gjithë përbërësit organikë, duke lënë një skelë minerale.
Pro:
Me furnizim të bollshëm dhe mund të formësohet lehtësisht.
Ofron një skelë të qëndrueshme për rritjen e kockave të reja.
Kundër:
Koha më e gjatë e integrimit pasi nuk ka qeliza të gjalla.
Potenciali për përgjigje imune (i rrallë).

Sintetike
Graftet sintetike janë materiale të prodhuara nga njeriu që imitojnë kockën natyrale.
Ato janë qeramika, polimere dhe qelqi bioaktiv.
Pro:
Asnjë transmetim i sëmundjes.
Mund të formohet në madhësi dhe forma specifike.
Kundër:
Normat e integrimit ndryshojnë në varësi të materialit.

Mungesa e vetive biologjike të kockave natyrale.
Aloplastike
Graftet aloplastike janë materiale sintetike për të mbushur defektet e kockave.
Shpesh përdoret në kombinim me graftet e tjera për të arritur rezultate më të mira.
Pro:
Plotësisht sintetike, pa rrezik transmetimi të sëmundjes.
Mund të personalizohet për nevojat e pacientit.
Kundër:
Integrimi varet nga faktorët material dhe të pacientit.
Përdoret si një suplement dhe jo si transplant primar.
| Lloji i Graftit | Burimi | Avantazhet | Konsideratat |
|---|---|---|---|
| Autotransformim | Trupi i vetë pacientit | Shkalla e lartë e suksesit, transmetimi i reduktuar i sëmundjes | Kërkon vendin e dytë kirurgjik, disponueshmëri e kufizuar |
| Alograft | Donator (njerëzor) | Asnjë operacion shtesë, i disponueshëm lehtësisht | Rreziku minimal i transmetimit të sëmundjes, integrimi më i ngadalshëm |
| Ksenograft | Kafshë (gjedhi) | Furnizimi i bollshëm, skela e qëndrueshme | Koha më e gjatë e integrimit, përgjigje e rrallë imune |
| Sintetike | Materiale të bëra nga njeriu | Asnjë transmetim i sëmundjes, i personalizueshëm | Integrimi i ndryshueshëm, i mungojnë vetitë biologjike |
| Aloplastike | Materiale sintetike | Eliminon rrezikun e sëmundjes, i përshtatur sipas nevojave | Varet nga vetitë e materialit, shpesh plotësuese |
Indikacionet për Shartimin e Kockave
Kocka e pamjaftueshme
Shartimi i kockave nevojitet kur nuk ka vëllim të mjaftueshëm kockor për të mbështetur implantet dentare me humbje kockore.
Kjo mund të jetë për shkak të arsyeve të ndryshme, të tilla si humbja e dhëmbëve, sëmundjet e mishrave të dhëmbëve ose sëmundjet kongjenitale.
Në këto raste, shartimi i kockave ndihmon në rritjen e kockës dhe siguron një platformë të qëndrueshme për vendosjen e implantit.
Pikat kryesore:
Suksesi i implantit dentar varet nga vëllimi dhe dendësia e mjaftueshme e kockave.
Kocka e pamjaftueshme mund të çojë në dështim ose komplikime të implantit.
Nxjerrja e dhëmbëve
Nxjerrja e dhëmbëve mund të çojë në humbje kockore me kalimin e kohës dhe të vështirësojë vendosjen e implanteve dentare.
Shartimi i kockave mund të bëhet menjëherë pas nxjerrjes për të ruajtur strukturën e kockës dhe për të lehtësuar vendosjen e implantit në të ardhmen.
Të mirat:
Parandalon resorbimin e kockave dhe ruan formën natyrale të nofullës.
Përmirëson rezultatin estetik të implanteve dentare.

Sëmundja periodontale
Sëmundja periodontale mund të shkaktojë humbje të konsiderueshme të kockave rreth dhëmbëve dhe të bëjë dhëmbët të lirohen dhe përfundimisht të bien.
Shartimi i kockave mund të rigjenerojë kockën e humbur dhe të stabilizojë dhëmbët.
Pikat kryesore:
Sëmundja periodontale prek jo vetëm mishrat, por edhe kockën e poshtme.
Shartimi i kockave mund të parandalojë humbjen e mëtejshme të dhëmbëve dhe shëndetin oral.

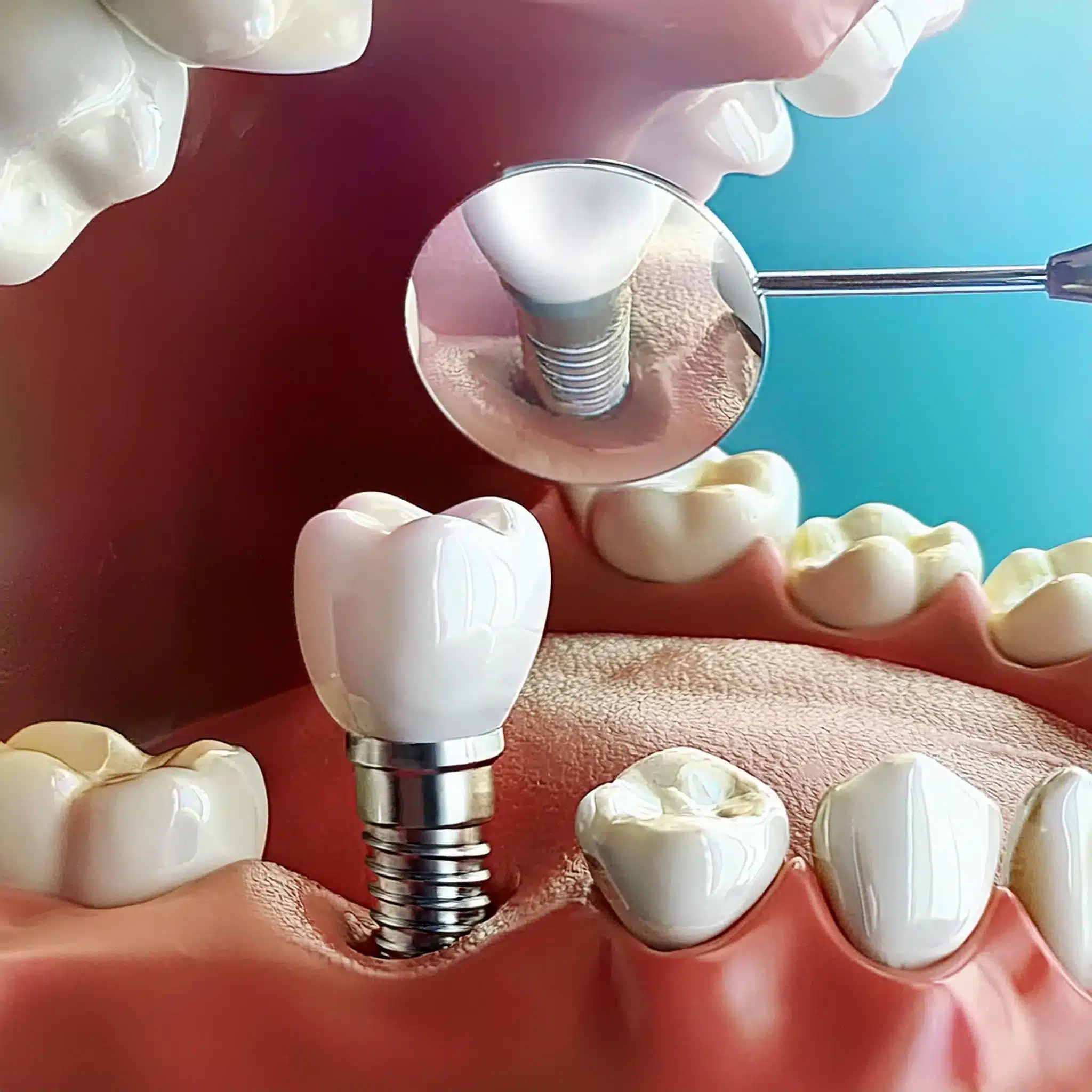
Implantet Dentare
Implantet dentare kanë nevojë për vëllim dhe densitet të mjaftueshëm kockor për integrim.
Shartimi i kockave shpesh kërkohet për pacientët me kocka të pamjaftueshme për të siguruar një bazë solide për implantet.
Disavantazhet:
Lloji dhe sasia e transplantit kockor varet nga pacienti individual.
Planifikimi dhe ekzekutimi i duhur i shartimit të kockave është vendimtar për suksesin e implantit.
| Indikacion | Përshkrimi | Konsideratat kryesore |
|---|---|---|
| Vëllimi i pamjaftueshëm i kockave | Shartimi i kockave është i nevojshëm kur ka vëllim të pamjaftueshëm kockor për të mbështetur implantet dentare. | Suksesi i implanteve dentare varet nga vëllimi dhe dendësia e duhur e kockave. |
| Nxjerrja e dhëmbëve | Shartimi i kockave mund të kryhet menjëherë pas nxjerrjes së dhëmbit për të ruajtur strukturën e kockave. | Parandalon resorbimin e kockave dhe ruan konturin natyral të nofullës. |
| Sëmundja periodontale | Shartimi i kockave mund të ndihmojë në rigjenerimin e kockave të humbura dhe stabilizimin e dhëmbëve. | Sëmundja periodontale prek jo vetëm mishrat e dhëmbëve, por edhe kockën e poshtme. |
| Implantet Dentare | Shartimi i kockave është shpesh një parakusht për pacientët me kockë joadekuate, duke siguruar një bazë të fortë për implantet. | Lloji dhe sasia e transplantit kockor të nevojshëm varet nga gjendja individuale e pacientit. |
Procedura dhe Rikuperimi
Para-op
Përgatitja para operacionit për shartimin e kockave përfshin disa hapa për të arritur rezultate të mira.
Pacientët duhet të informojnë dentistin e tyre për të gjitha medikamentet që po marrin, pasi disa mund të ndikojnë në procesin e shërimit.
Restaurimet ekzistuese mund të kenë nevojë të rregullohen për të akomoduar transplantin.
Një dietë e butë, e butë dhe e ekuilibruar nga ana ushqyese për 2-4 ditë (ose më gjatë nëse është e nevojshme) pas operacionit për të ndihmuar rikuperimin.
Këshilla para operacionit:
Informoni dentistin tuaj për të gjitha medikamentet.
Rregulloni restaurimet ekzistuese nëse është e nevojshme.
Planifikoni një dietë të butë pas operacionit.

Procedura kirurgjikale
Procedura kirurgjikale për shartimin e kockave përfshin:
Anestezia: Anestezia lokale për të mpirë zonën.
Nxjerrja dhe/ose burimi i kockave: Nxjerrja e dhëmbit (nëse nevojitet) dhe sigurimi i materialit të transplantit të kockave.
Futja e graftit: Futja e graftit kockor në defekt.
Qepje: mbyllja e vendit të prerjes me qepje.
Hapat kirurgjikale:
-
Anestezia për lehtësimin e dhimbjeve.
-
Nxjerrja dhe sigurimi i materialit të shartimit.
-
Futja e graftit kockor.
-
Qepje për të mbyllur prerjen.

Kujdesi pas operacionit
Kujdesi pas operacionit është i rëndësishëm për të siguruar shërimin e duhur dhe komplikimet minimale.
Pacientët duhet të ndjekin një dietë të butë, të shmangin aktivitetet e rënda dhe të kenë higjienë të mirë orale.
Ndjekja e rregullt me dentistin për të monitoruar shërimin dhe për të hequr qepjet.
Pas operacionit:
Dietë e butë për 2-4 ditë.
Shmangni aktivitetet e forta.
Higjienë e mirë orale.
Vazhdoni takimet.

Rreziqet dhe komplikimet
Shartimi i kockave, si çdo procedurë kirurgjikale, ka rreziqe dhe komplikime.
Është e rëndësishme t'i kuptoni këto për të marrë vendime të informuara për shëndetin tuaj.
Rreziqet dhe komplikimet e zakonshme
Infeksioni: Infeksioni është një rrezik i zakonshëm i shartimit të kockave.
Kjo mund të ndodhë në vendin e donatorit ose në vendin e marrësit dhe mund të kërkojë trajtim shtesë.
Gjakderdhje: Gjakderdhja gjatë operacionit është një tjetër rrezik.
Në disa raste, kjo mund të kërkojë një transfuzion gjaku.
Problemet e shërimit të kockave: Kocka e shartuar mund të mos shërohet siç duhet dhe mund të çojë në komplikime të tilla si mos bashkim ose bashkim i keq.
Dhimbje kronike: Disa pacientë mund të përjetojnë dhimbje kronike në vendin e transplantimit.
Frakturat: Ekziston rreziku i frakturave në vendin e transplantit, veçanërisht nëse kocka nuk shërohet siç duhet.
Dështimi i harduerit: Nëse përdoren pajisje si pllaka dhe vida, ekziston rreziku i dështimit të harduerit.

Përfundim & Çështje kryesore
Pikat kryesore:
Shartimi i kockave është një procedurë kyçe për trajtimet dentare dhe ortopedike.
Llojet e ndryshme të graftit kockor (autograft, alograft, ksenograft, sintetik, aloplastik) kanë avantazhet dhe disavantazhet e tyre.
Njohja e indikacioneve, procedurave dhe rreziqeve është e rëndësishme për një vendim të informuar.
konkluzioni
Shartimi i kockave përdoret në shumë trajtime mjekësore si bazë për implantet dentare dhe për të trajtuar defektet e kockave. Duke ditur llojet e ndryshme të transplanteve, indikacionet, rreziqet dhe komplikimet e tyre, pacientët mund të marrin vendime të informuara.
FAQ
Referencat
Esposito M, Grusovin MG, Coulthard P, et al. Ndërhyrjet për zëvendësimin e dhëmbëve që mungojnë: implantet dentare në foletë ekstraktuese të freskëta. Cochrane Database Syst Rev. 2006;(3):CD005968.
Neni: Ndërhyrjet për zëvendësimin e dhëmbëve që mungojnë: implantet dentare në foletë ekstraktuese të freskëtaPanchal M, Khare S, Khamkar P, etj. Implantet dentare: Një përmbledhje e llojeve, analizave të dizajnit, materialeve, metodave të prodhimit të aditivëve dhe fushëveprimit në të ardhmen. Procedura CIRP. 2022; 105: 214-219.
Neni: Implantet dentare: Një përmbledhje e llojeve, analizave të dizajnit, materialeve, metodave të prodhimit të aditivëve dhe qëllimit të ardhshëmGuillaume B. Implantet dentare: Një përmbledhje. Morfologjia. 2016;100(329):189-198.
Neni: Implantet dentare: Një përmbledhjeAlbrektsson T, Zarb G, Worthington P, etj. Efikasiteti afatgjatë i implanteve dentare të përdorura aktualisht: një rishikim dhe kriteret e propozuara të suksesit. Implantet Maxillofac Oral Int J. 1986; 1 (1): 11-25.
Neni: Efikasiteti afatgjatë i implanteve dentare të përdorura aktualisht: një rishikim dhe kriteret e propozuara të suksesitMisch CE, Qu Z, Bidez MW. Vetitë mekanike të kockës trabekulare në mandibulën e njeriut: implikimet për planifikimin e trajtimit të implantit dentar dhe vendosjen kirurgjikale. J Oral Maxillofac Surg. 1999; 57 (6): 700-706.
Neni: Vetitë mekanike të kockës trabekulare në mandibulën e njeriut: implikimet për planifikimin e trajtimit të implantit dentar dhe vendosjen kirurgjikaleLindhe J, Meyle J. Sëmundjet peri-implantare: Raporti konsensus i seminarit të gjashtë evropian mbi periodontologjinë. J Clin Periodontol. 2008; 35 (8 Suppl): 282-285.
Neni: Sëmundjet peri-implantare: Raporti konsensus i Punëtorisë së Gjashtë Evropiane mbi Periodontologjinë