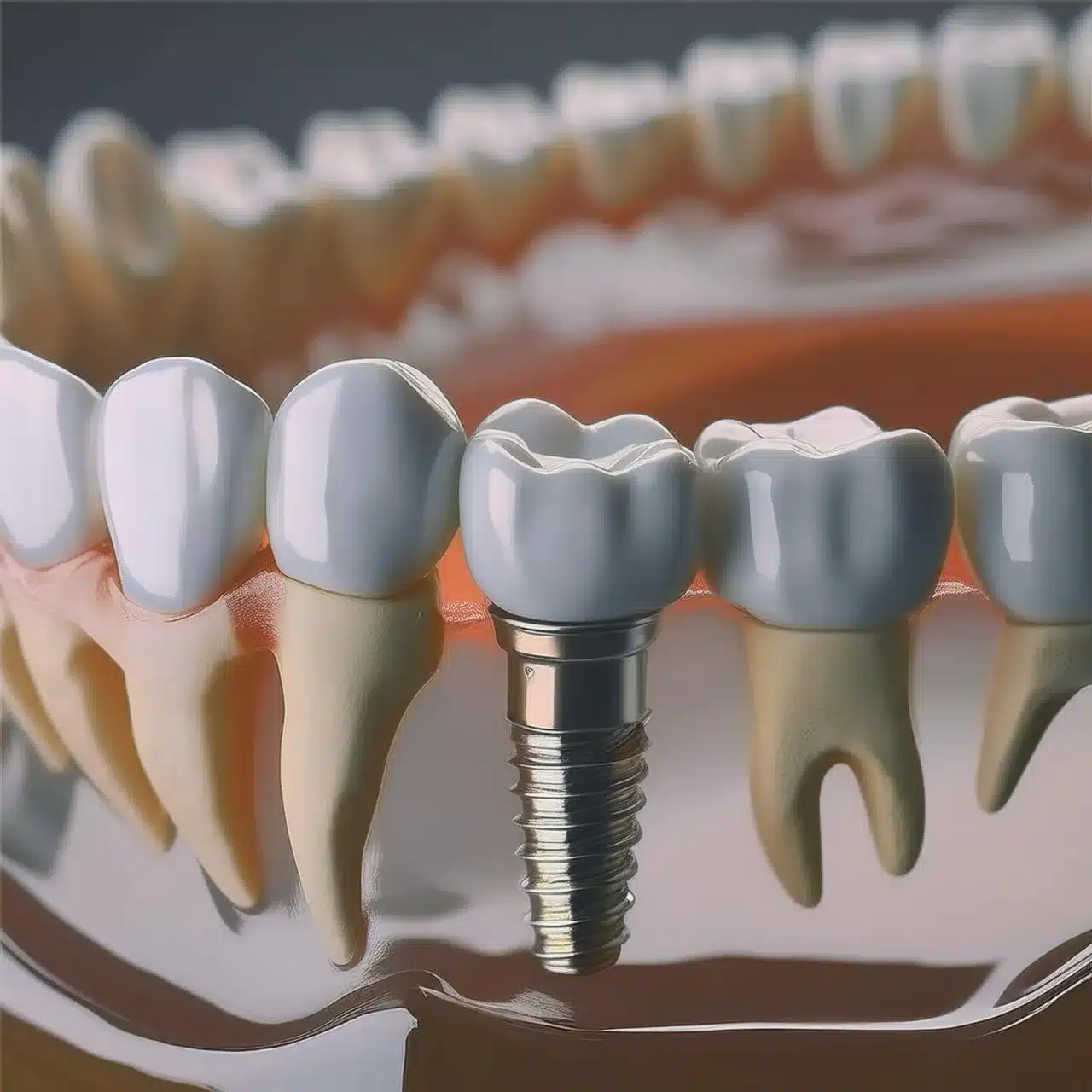
Oseointegrimi i implantet dentare është çelësi i suksesit afatgjatë të restaurimit tuaj dentar.
Nëse po konsideroni implantet dentare, me siguri po pyesni veten se si ato ngjiten në kockën e nofullës tuaj, çfarë ndikon në stabilitetin e tyre dhe si të merrni një rezultat të mirë.
Çfarë është osseointegrimi i implanteve dentare?
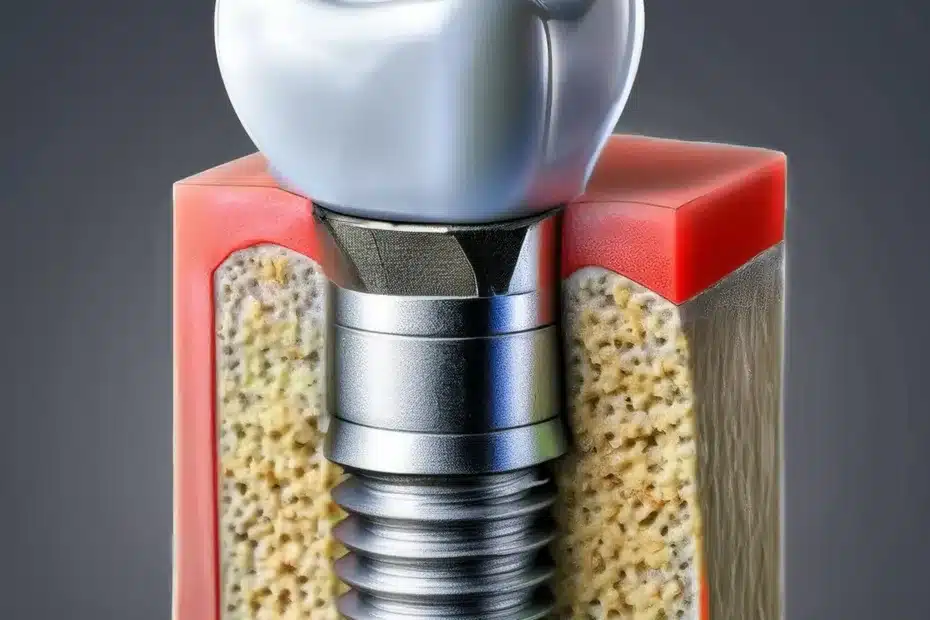
Oseointegrimi i implanteve dentare është procesi biologjik ku qelizat kockore rriten në sipërfaqen e implantit, duke formuar një lidhje të drejtpërdrejtë me kockën e nofullës. Ky proces zgjat 3-6 muaj dhe është vendimtar për stabilitetin e implantit. Faktorët që ndikojnë në suksesin përfshijnë materialin e implantit, karakteristikat e sipërfaqes, cilësinë e kockave dhe shëndetin e pacientit. Oseointegrimi i suksesshëm kontribuon në shkallën e suksesit afatgjatë të implantit deri në 95%.

Procesi i Oseointegrimit
Oseointegrimi është një proces biologjik që siguron që implanti dentar të jetë i qëndrueshëm në kockën e nofullës.
Ky proces ka disa faza, secila kritike për suksesin afatgjatë të implantit.
Faza fillestare e shërimit
Menjëherë pas vendosjes së implantit dentar fillon faza fillestare e shërimit.
Pas operacionit të implantit dentar, trupi e sheh implantin si një objekt të huaj dhe fillon një proces shërimi që është thelbësor për osteointegrimin.
Reagimi inflamator: Trupi fillon një përgjigje inflamatore, një pjesë e natyrshme e procesit të shërimit.
Kjo fazë zgjat disa ditë dhe është e rëndësishme për largimin e mbetjeve dhe baktereve nga vendi i kirurgjisë.
Formimi i mpiksjes: Një mpiksje gjaku formohet rreth implantit, një skelë për rritjen e indeve të reja.
Ky mpiksje është thelbësor për stabilizimin e implantit dhe për rritjen e qelizave të reja kockore (1).

Fiksimi biologjik dhe rimodelimi i kockave
Ndërsa shërimi përparon, ndodh fiksimi biologjik i implantit.
Kjo fazë është vendi ku implanti integrohet me kockën përreth.
Rritja e qelizave kockore: Osteoblastet, qelizat që formojnë kocka, fillojnë të rriten në sipërfaqen e implantit për një lidhje të fortë.
Ky proces lehtësohet nga vetitë e sipërfaqes së implantit, të cilat mund të optimizohen përmes trajtimeve specifike (3).
Rimodelimi i kockave: Me kalimin e kohës, kocka rimodelohet për t'u përshtatur me ngarkesat mekanike në implant.
Ky rimodelim është kritik për stabilitetin dhe funksionin afatgjatë të implantit (5).

Oseointegrimi për suksesin e implantit dentar
Oseointegrimi është çelësi i suksesit të implanteve dentare, që implantet të jenë funksionale dhe të qëndrueshme në afat të gjatë.
Stabiliteti dhe jetëgjatësia
Stabiliteti i një implanti dentar varet nga osseointegrimi.
Integrimi afatgjatë: Oseointegrimi i suksesshëm do të thotë se implanti është i ankoruar në kockën e nofullës, duke reduktuar rrezikun e lëvizshmërisë ose dështimit me kalimin e kohës (1).
Kënaqësia e pacientit: Një implant i qëndrueshëm nënkupton kënaqësi më të lartë të pacientit pasi ndihet dhe funksionon si dhëmbët natyralë, duke lejuar aktivitete normale të përtypjes dhe të folurit (1).
Ruajtja e kockave
Oseointegrimi është i rëndësishëm për shëndetin e kockave.
Parandalimi i humbjes së kockave: Implantet e integruara mirë ndihmojnë në ruajtjen e kockës duke ofruar stimulimin e nevojshëm për të parandaluar resorbimin e kockave, një problem i zakonshëm me mungesën e dhëmbëve (2).

Shëndeti i përgjithshëm oral
Osteointegrimi ndikon në shëndetin e përgjithshëm oral.
Rreziku i reduktuar i infeksionit: Një implant i integruar mirë zvogëlon boshllëqet ku mund të grumbullohen bakteret, duke reduktuar rrezikun e infeksionit dhe inflamacionit (3).
Mbështetje për dhëmbët ngjitur: Implantet e osteointegruara mbështesin dhëmbët ngjitur, duke i penguar ata të lëvizin dhe duke siguruar një kafshim të ekuilibruar (3).
Faktorët që Ndikojnë në Oseointegrimin
Kuptimi i faktorëve që ndikojnë në osseointegrimin është i rëndësishëm për suksesin e implantit dentar.
Këta faktorë mund të ndahen në ndikime implantare, pacienti dhe procedurale.
Materiali dhe sipërfaqja e implantit
Materiali dhe sipërfaqja e implanteve dentare janë të rëndësishme për osteointegrimin.
Materiali: Titani dhe lidhjet e tij përdoren për shkak të biokompatibilitetit dhe vetive mekanike që lejojnë integrimin e kockave (6).
Vrazhdësia e sipërfaqes: Implantet me topografi sipërfaqësore të përafërt janë treguar se përmirësojnë ngjitjen dhe rritjen e qelizave kockore, duke rezultuar në osseointegrim më të mirë (4).
Modifikimet e sipërfaqes: Teknika të tilla si gravurja me acid dhe spërkatja me plazmë mund të përmirësojnë më tej sipërfaqen për integrim më të mirë të kockave (5).

Shëndeti dhe mënyra e jetesës së pacientit
Shëndeti i përgjithshëm dhe mënyra e jetesës së pacientit ndikojnë në osseointegrimin.
Kushtet sistematike shëndetësore: Kushtet si diabeti dhe osteoporoza mund të pengojnë shërimin dhe integrimin e kockave dhe kërkojnë menaxhim dhe monitorim të kujdesshëm (6).
Mënyra e jetesës: Pirja e duhanit dhe higjiena e dobët orale mund të ndikojnë në osseointegrimin, pasi mund të shkaktojë inflamacion dhe shërim të vonuar (3).
Statusi i të ushqyerit: Ushqimi adekuat, veçanërisht kalciumi dhe vitamina D, mbështet shëndetin e kockave dhe integrimin kockor (2).
| Faktori | Përshkrimi | Ndikimi në Osseointegrimin |
|---|---|---|
| Materiali i implantit | Titani dhe lidhjet e tij preferohen për shkak të biopërputhshmërisë së tyre të shkëlqyer dhe vetive mekanike. | Lehtëson integrimin e kockave (6) |
| Topografia sipërfaqësore | Sipërfaqet e vrazhda përmirësojnë lidhjen dhe rritjen e qelizave kockore. | Përmirëson rezultatet e osteointegrimit (4) |
| Shëndeti i pacientit | Kushtet sistematike shëndetësore si diabeti dhe osteoporoza mund të ndikojnë në shërimin e kockave dhe integrimin kockor. | Kërkon menaxhim dhe monitorim të kujdesshëm (6) |
| Zgjedhjet e stilit të jetesës | Pirja e duhanit dhe higjiena e dobët e gojës ndikojnë negativisht në osseointegrimin. | Çon në inflamacion dhe shërim të vonuar (3) |
| Teknika kirurgjikale | Saktësia në vendosjen e implantit dhe trauma minimale në indet përreth janë thelbësore. | Përmirëson osseointegrimin dhe zvogëlon kohën e shërimit (2) |
Teknika kirurgjikale dhe kujdesi pas kirurgjisë
Teknika kirurgjikale dhe kujdesi postkirurgjik janë të rëndësishme për osseointegrimin.
Saktësia në vendosje: Vendosja e saktë e implantit me trauma minimale të indeve është çelësi i integrimit (2).
Protokollet pas kirurgjisë: Ndiqni kujdesin e rekomanduar pas operacionit, duke përfshirë higjienën orale dhe pa stres në implant, për osseointegrim të suksesshëm (1).
Protokollet e ngarkimit: Protokollet e ngarkimit të menjëhershëm ose të vonuar duhet të zgjidhen bazuar në stabilitetin e pacientit dhe implantit, pasi mund të ndikojë në shërimin (2).
Sfidat dhe zgjidhjet në Osseointegrim
Oseointegrimi është i rëndësishëm, por mund të përballet me disa sfida që mund të pengojnë integrimin e implantit dentar.
Kuptimi i këtyre sfidave dhe zgjidhjeve të tyre është i rëndësishëm për rezultate më të mira të implantit.
Dendësia e pamjaftueshme e kockave
Një nga sfidat më të mëdha në osseointegrimin është densiteti i pamjaftueshëm i kockave që mund të rrezikojë stabilitetin e implantit.
Cilësia e kockave: Cilësia e dobët e kockave nuk mund të mbështesë implantin, duke rritur rrezikun e dështimit (1).
Teknikat e vlerësimit: Teknika të avancuara imazherike, të tilla si skanimet CT, nevojiten për të vlerësuar densitetin e kockës përpara implantimit për të planifikuar trajtimin siç duhet (2).

Shartimi i kockave
Shartimi i kockave është një zgjidhje për densitetin e pamjaftueshëm të kockave për të rritur shanset e osseointegrimit.
Autotransplantet dhe alograftet: Këto janë llojet më të zakonshme të transplanteve të kockave që përdoren për të shtuar volumin e kockave për të mbështetur implantet (3).
Normat e suksesit: Studimet tregojnë se shartimi i kockave mund të përmirësojë shkallët e suksesit të implantit në zona me cilësi të dobët të kockave, deri në 90% (4).
Komplikimet
Kontrolli i infeksionit: Teknika strikte aseptike gjatë operacionit dhe kujdesit postkirurgjik është e rëndësishme për të parandaluar infeksionin që mund të prishë osseointegrimin (5).
Monitorimi dhe ndjekja: Ndjekja e rregullt është e rëndësishme për të monitoruar vendin e implantit për çdo ndërlikim dhe për të ndërhyrë herët (6).
Të Procesi dhe afati kohor i implantit dentar hap pas hapi përfshin disa faza, duke përfshirë vendosjen e implantit, shërimin dhe osseointegrimin, vendosjen e abutmentit dhe montimin e kurorës.

Çdo fazë është kritike për suksesin afatgjatë të implantit.
Procesi fillon me futjen kirurgjikale të shtyllës së implantit në kockën e nofullës, e ndjekur nga një fazë shërimi ku implanti integrohet me kockën.
Pasi shërimi të përfundojë, mbështetësja ngjitet dhe kurora e bërë me porosi vendoset në abutment.
Ky proces siguron që implanti dentar të jetë i qëndrueshëm dhe funksional, duke siguruar një zëvendësim të dhëmbëve me pamje natyrale dhe ndjesi.
Përfundim & Çështje kryesore
Merr kryesore:
Oseointegrimi është i rëndësishëm: Integrimi i implanteve dentare në kockën e nofullës, osseointegrimi, është i rëndësishëm për stabilitetin dhe funksionalitetin afatgjatë të implantit.
Faktorë të Shumëfishtë: Materiali i implantit, topografia e sipërfaqes, shëndeti i pacientit dhe teknika kirurgjikale ndikojnë në osseointegrimin.
Sfidat mund të zgjidhen: Sfidat si densiteti i pamjaftueshëm i kockave mund të zgjidhen përmes shartimit të kockave për të rritur shanset për sukses.
konkluzioni:
Oseointegrimi është çelësi i implantologjisë së suksesshme dentare.
Duke kuptuar dhe zgjidhur faktorët dhe sfidat, profesionistët dentarë mund të përmirësojnë rezultatet e pacientit dhe implantet do të jenë të sigurta dhe funksionale për shumë vite.

FAQ
Referencat
Albrektsson T, Zarb G, Worthington P, etj. Efikasiteti afatgjatë i implanteve dentare të përdorura aktualisht: një rishikim dhe kriteret e propozuara të suksesit. Implantet Maxillofac Oral Int J. 1986; 1:11-25.
Neni: Efikasiteti afatgjatë i implanteve dentare të përdorura aktualisht: një rishikim dhe kriteret e propozuara të suksesitEsposito M, Grusovin MG, Chew YS, et al. Vendosja e implantit me një fazë kundrejt dy fazave. Një përmbledhje sistematike e Cochrane e sprovave klinike të kontrolluara të rastësishme. Eur J Implantol Oral. 2009; 2:91-9.
Neni: Vendosja e implantit me një fazë kundrejt dy fazaveStanford CM, Keller JC, Solursh M. Shprehja e qelizave kockore në sipërfaqet e titanit ndryshohet nga trajtimet e sterilizimit. J Dent Res. 1994; 73: 1061-71.
Neni: Shprehja e qelizave kockore në sipërfaqet e titanit ndryshohet nga trajtimet e sterilizimitSchwartz Z, Boyan BD. Mekanizmat themelorë në ndërfaqen kockë-biomaterial. J Cell Biochem. 1994; 56: 340-7.
Neni: Mekanizmat themelorë në ndërfaqen kockë-biomaterialBoyan BD, Hummert TW, Dean DD, et al. Roli i sipërfaqeve materiale në rregullimin e përgjigjes së qelizave të kockave dhe kërcit. Biomaterialet. 1996; 17:137-46.
Neni: Roli i sipërfaqeve materiale në rregullimin e përgjigjes së qelizave të kockave dhe kërcitCaplan AI. Qelizat staminale mezenkimale. J Orthop Res. 1991; 9: 641-50.
Neni: Qelizat staminale mezenkimale