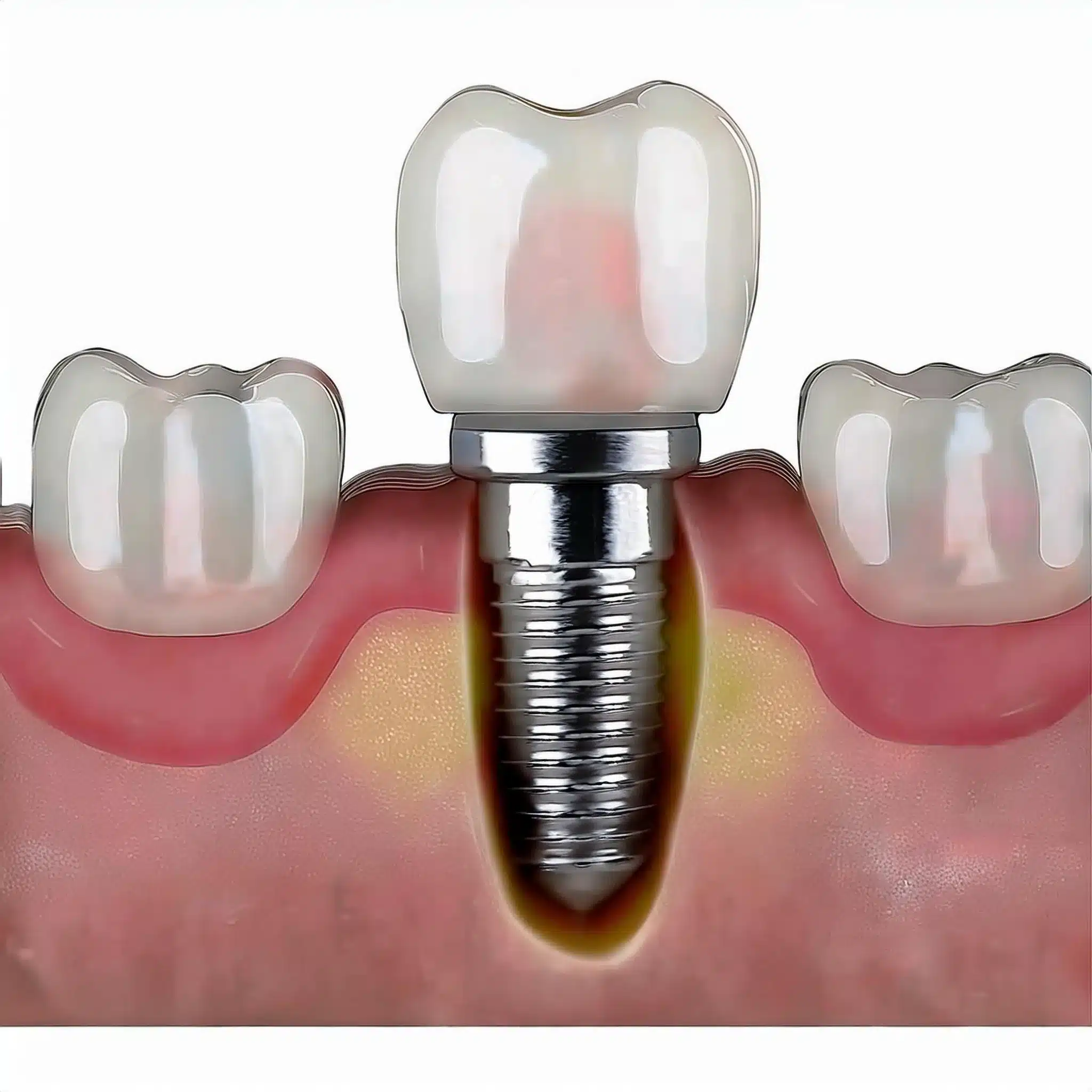
Peri-implantitis, the nemesis of dental implants, is a big worry for those who have invested in this life-changing procedure.
If you’re experiencing inflammation, bleeding, or pain around your dental implant, you’re probably wondering what’s causing this and how to stop it from getting worse.
What is Peri-implantitis?
Peri-implantitis is an inflammatory condition around the dental implant that causes bone loss and potential implant failure. It’s mainly caused by bacterial infections, poor oral hygiene, and systemic conditions like diabetes. Early diagnosis is key, with treatment options including mechanical debridement, antiseptic treatment, and, in some cases, surgical intervention.

Causes of Peri-implantitis
Bacterial Infection
Peri-implantitis poses a significant threat to the longevity of dental implants, leading to potential Dental Implant Failure and Rejection if left untreated.
The main cause of peri-implantitis is bacterial accumulation around the implant.
This infection causes inflammation and progressive bone loss but also poses significant risks and complications that threaten the stability of the implant.
Studies have shown that bacterial biofilms are key to the pathogenesis of peri-implantitis as they trigger an immune response that results in tissue destruction (1).
Poor Oral Hygiene
Poor oral care can lead to plaque and infection and increase the risk of peri-implantitis.
Regular and good oral hygiene is essential to prevent bacterial accumulation and keep the tissues around the implant healthy (2).

Systemic Conditions
Systemic conditions like diabetes can increase the risk of peri-implantitis.
These conditions can impair the body’s ability to fight infections and make it more susceptible to inflammation and bone loss around the implant (3).
Smoking
Smoking is a major risk factor for peri-implantitis.
Smoking affects blood flow and immune response and can compromise healing and increase the risk of infection and inflammation around the implant site (4).
| Risk Factor | Description |
|---|---|
| Bacterial Infection | Accumulation of bacterial biofilms around the implant, leading to inflammation and bone loss(1). |
| Poor Oral Hygiene | Inadequate oral care resulting in plaque buildup and increased risk of infection(2). |
| Systemic Conditions | Conditions like diabetes that impair the body’s ability to fight infections, increasing susceptibility to peri-implantitis(3). |
| Smoking | Tobacco use affects blood flow and immune response, compromising healing and increasing the likelihood of infection(4). |
Symptoms of Peri-implantitis
Inflammation
Peri-implantitis starts with inflammation, manifesting as redness and swelling around the implant site.
This initial symptom is a response to bacterial biofilm accumulation and, if not addressed, can lead to further complications (2).
Bleeding
Bleeding on probing or spontaneously is a sign of peri-implantitis.
This means there’s inflammation and infection in the peri-implant tissues, which, if left untreated, can progress to more severe conditions (3).
Bone Loss
One of the most worrying symptoms of peri-implantitis is the progressive loss of supporting bone structure.
This bone loss is often non-linear and can accelerate if the underlying causes are not managed well.
It’s important to monitor bone levels regularly to prevent implant failure (4).

Discomfort
Patients with peri-implantitis may experience pain or discomfort around the implant site.
This discomfort can be mild to severe and often correlates with the degree of inflammation and bone loss.
Addressing this symptom early can stop the disease from progressing (5).
If you notice these symptoms early and get professional dental care, the prognosis is better for patients with peri-implantitis.
Regular monitoring and maintenance are key to managing these symptoms and keeping the dental implants healthy.
Diagnosis of Peri-implantitis
Clinical Examination
The diagnosis of peri-implantitis involves a clinical examination to look for signs of inflammation and bleeding.
This includes bleeding on probing and/or suppuration, increased probing depths and recession of the peri-implant mucosa (3 depths).
Radiographic Analysis
Radiographs are used to assess bone levels around the implant.
This helps to identify marginal bone loss, which is a sign of peri-implantitis.
Regular radiographs can monitor bone loss and guide treatment (4).
Probing Depth Measurement
Measuring the depth of the pockets around the implant is important for diagnosing peri-implantitis.
Increased probing depths compared to previous examination mean there’s inflammation and infection.
This measurement helps to determine the severity of the condition and treatment plan (5).

Diagnostic Criteria
Peri-implantitis can be diagnosed based on clinical criteria, which includes peri-implant signs of inflammation, bleeding, and/or suppuration on gentle probing and increased probing depths.
These criteria helps to differentiate peri-implantitis from other conditions and to intervene early (6).
Treatment of Peri-implantitis
Non-Surgical Treatment
Non-surgical treatment for peri-implantitis includes mechanical debridement and antiseptic treatment.
These methods aims to remove bacterial biofilms and reduce inflammation to prevent further bone loss and promote healing.
Studies have shown that non-surgical treatment can be effective in managing peri-implantitis, especially when combined with regular dental check-ups and good oral hygiene habits (2).

Surgical Treatment
Surgical treatment may be needed for more advanced cases of peri-implantitis.
This involves flap surgery to clean and regenerate bone around the implant.
Surgical treatment aims to remove infected tissue, decontaminate the implant surface and promote bone regeneration.
Research has shown that surgical treatment can be effective in treating peri-implantitis, especially when combined with antibiotic treatment and good postoperative care (3).
Antibiotic Treatment
Antibiotic treatment is often used as an adjunct to periimplantitis treatment.
Systemic or local antibiotics can control infection and reduce inflammation.
The choice of antibiotic depends on the severity of the infection and the patient’s overall health.
Research has shown that antibiotic treatment can be effective in managing peri-implantitis, especially when combined with non-surgical or surgical treatment (4).
Laser Treatment
Laser treatment is another option for peri-implantitis.
Lasers can remove infected tissue and promote healing.
Research has shown that laser treatment can reduce inflammation and bone fill in peri-implantitis defects (5).
| Treatment Option | Description |
|---|---|
| Non-Surgical Treatment | Mechanical debridement and antiseptic treatment to remove bacterial biofilms and reduce inflammation(2). |
| Surgical Intervention | Flap surgery to clean and regenerate bone around the implant, often combined with antibiotic therapy(3). |
| Antibiotic Therapy | Systemic or local antibiotics to control infection and reduce inflammation, often used as an adjunctive treatment(4). |
| Laser Therapy | Use of lasers to remove infected tissue and promote healing, effective in reducing inflammation and promoting bone fill in peri-implantitis defects(5). |
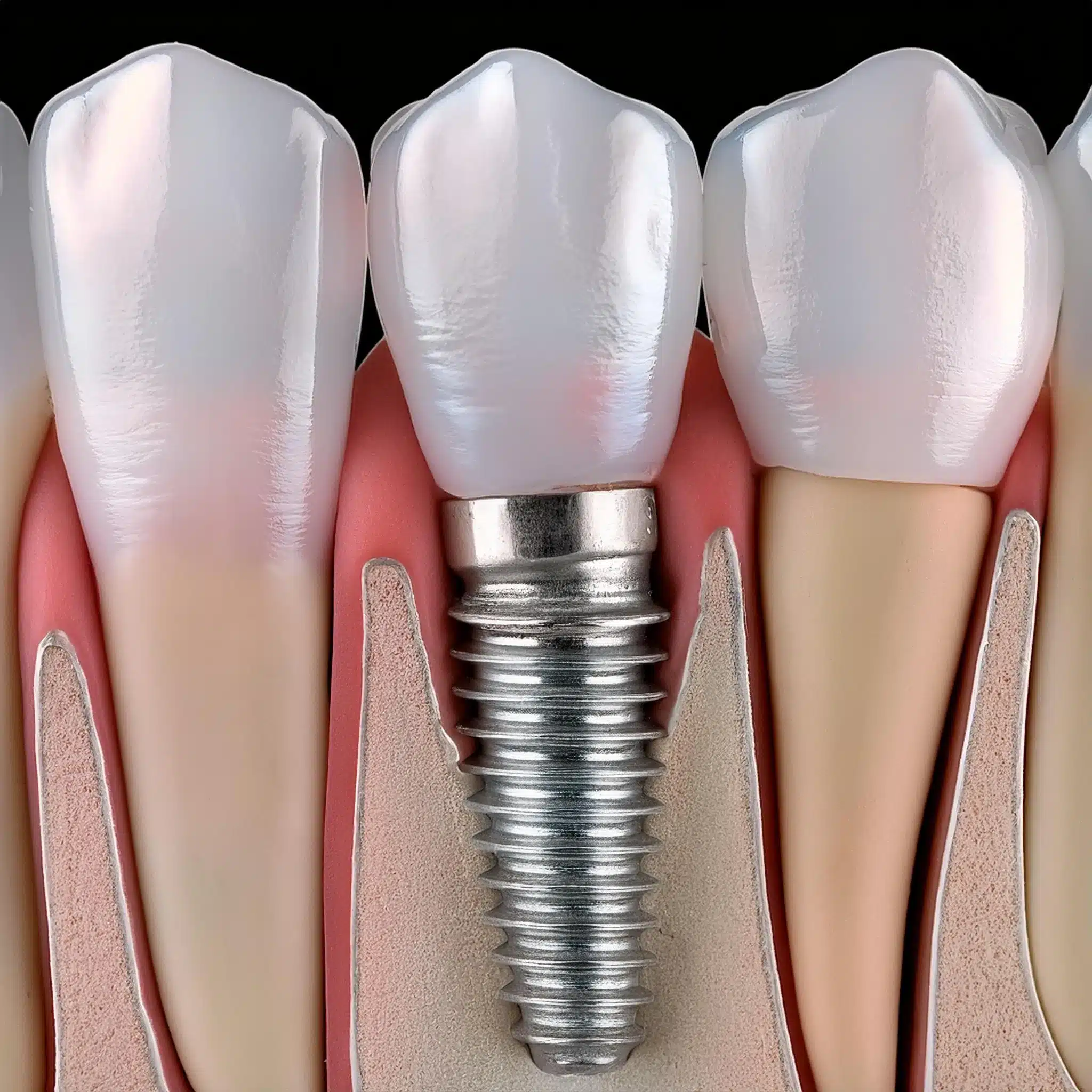
Prevention of Peri-implantitis
Regular Dental Check-ups
Regular dental check-ups is key to monitoring implant health and preventing peri-implantitis.
These visits allows early detection of any signs of inflammation or infection and intervene early to prevent further complications (1).
Good Oral Hygiene
Good brushing and flossing habits are important to maintain the health of the tissues around dental implants.
Good oral hygiene practices can prevent bacterial accumulation and reduce the risk of peri-implantitis (2).

Lifestyle Modifications
Lifestyle modifications, such as quitting smoking and managing systemic health conditions like diabetes, can reduce the risk of peri-implantitis.
These modifications can improve overall health and reduce complications with dental implants (3).
Professional Maintenance
Professional maintenance, including regular cleaning and debridement, is important to prevent peri-implantitis.
This will remove bacterial biofilms and reduce inflammation to preserve the health of the implant and surrounding tissues (4).

Conclusion & Key-Takeaways
Key-Takeaways
Peri-implantitis is preventable and treatable with early detection and treatment.
Good oral hygiene and regular dental check-ups are key to preventing peri-implantitis.
Know the causes, symptoms, and treatment of peri-implantitis if you have dental implants.
Conclusion
Peri-implantitis is a big threat to dental implants, but with proper care and early intervention, it can be managed.
By having regular dental check-ups and good oral hygiene, you can reduce the risk of peri-implantitis and ensure the long-term success of your dental implants.
FAQ
References
Renvert S, Polyzois I. Etiology, pathogenesis and treatment of peri-implantitis: A European consensus. J Clin Periodontol. 2024;51:123-130.
Article: Etiology, pathogenesis and treatment of peri-implantitis: A European consensusHeitz-Mayfield LJ, Mombelli A. Peri-implantitis: the beginning of the end for osseointegration? Periodontol 2000. 2014;66:251-269.
Article: Peri-implantitis: the beginning of the end for osseointegration?Schwarz F, Derks J, Monje A, Wang HL. Peri-implantitis. J Clin Periodontol. 2018;45(Suppl 20):S246-S266.
Article: Peri-implantitisLindhe J, Meyle J. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35(Suppl 8):282-285.
Article: Peri-implant diseases: Consensus Report of the Sixth European Workshop on PeriodontologyFiguero E, Graziani F, Sanz I, Herrera D, Sanz M. Management of peri-implant mucositis and peri-implantitis. Periodontol 2000. 2014;66:255-273.
Article: Management of peri-implant mucositis and peri-implantitisKlinge B, Meyle J. Peri-implant tissue destruction. The Third EAO Consensus Conference 2012. Clin Oral Implants Res. 2012;23(Suppl 6):108-110.
Article: Peri-implant tissue destruction. The Third EAO Consensus Conference 2012
