Thinking of replacing missing teeth with dental implants but worried about allergies or complications? Learn the pros and cons to make an informed decision about your mouth.
What is an Allergy to Dental Implants?
Dental implants allergy is an immune system response to titanium or other metals used in dental implants, affecting approximately 0.6% of patients. This condition can manifest through symptoms like swelling, pain, skin rashes, eczema, bone loss, or implant failure. While rare, it occurs more frequently in patients with previous metal allergies

Causes of Allergy to Dental Implants
Dental implants are generally safe but understanding the causes of allergies is key to proper treatment planning.
Materials Used in Dental Implants
Materials used in dental implants can cause allergic reactions.
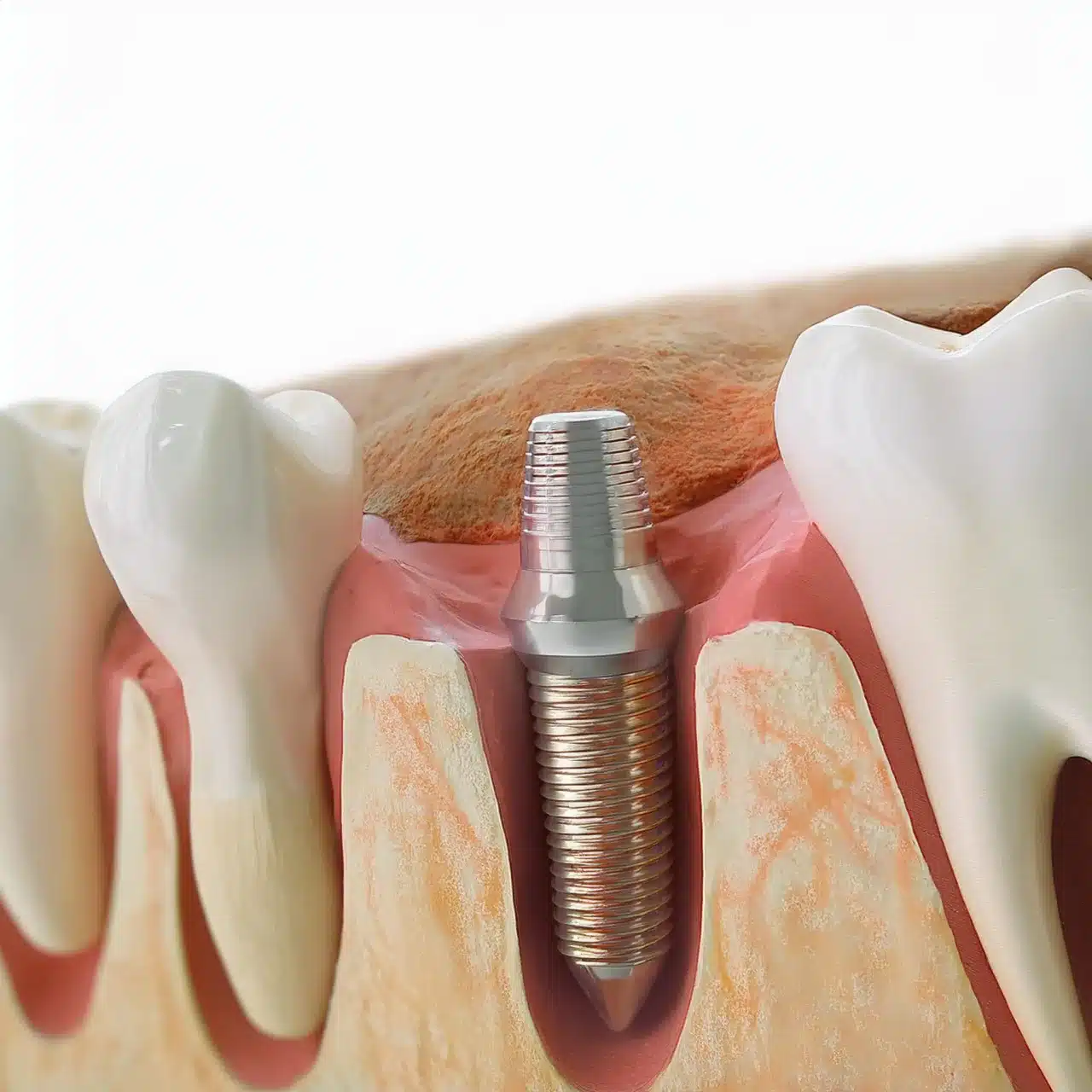
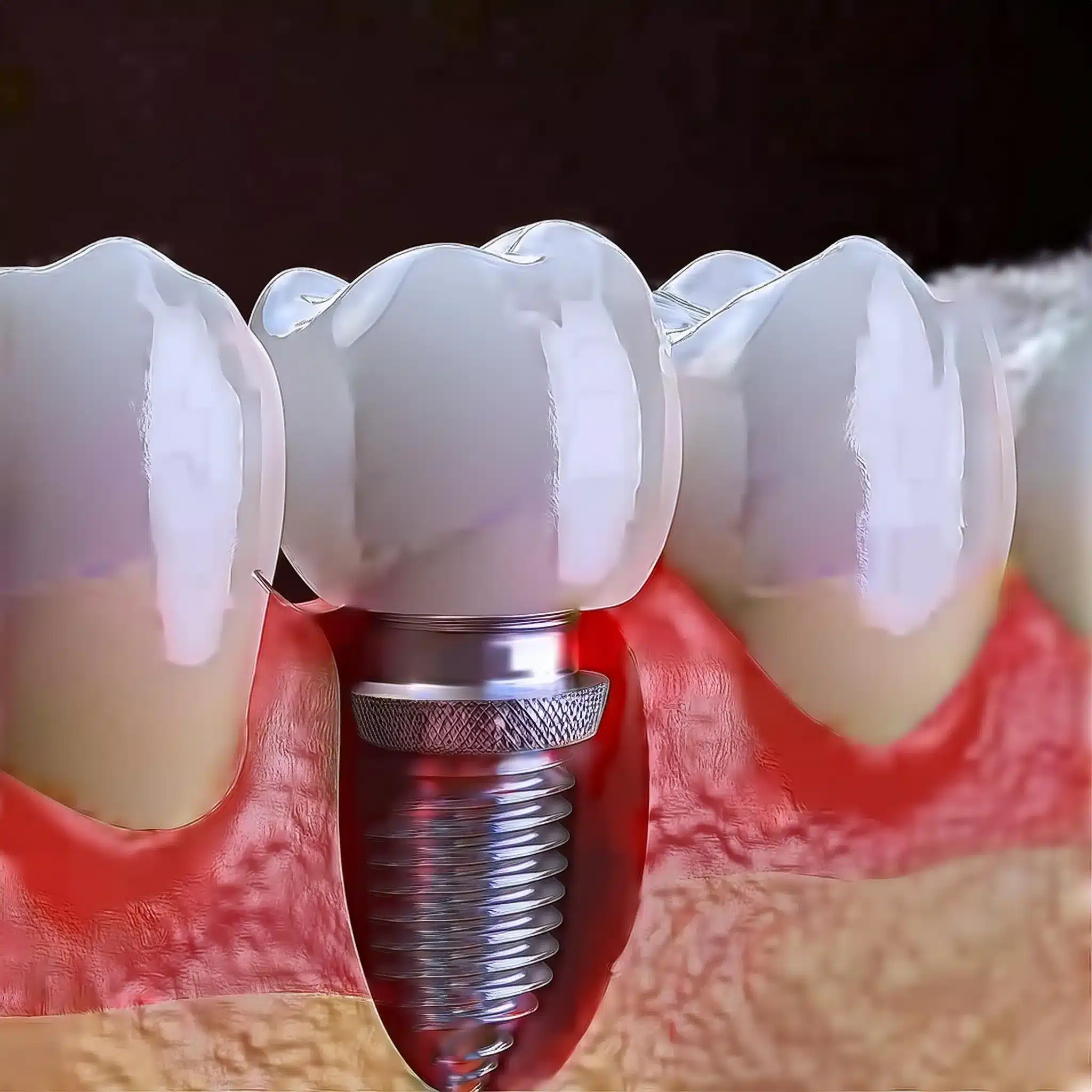
Titanium and Alloys: Titanium is used widely due to its biocompatibility but some individuals may still have allergies. Studies show titanium implants have high success rate but rough surfaces can increase risk of complications like peri-implantitis (1)
Alternative Materials: Other materials like zirconia and ceramics are being explored for its hypoallergenic properties. These materials aim to reduce risk of allergies while maintaining durability and effectiveness (2)
Immune System Response
The body’s immune response is key to allergic reactions to dental implants.
Inflammatory Reactions: The immune system reacts to the implant materials and causes inflammation and discomfort. This is more of a concern with rough surfaced implants which have been linked to higher risk of peri-implantitis (1)
Osseointegration: Successful osseointegration where the implant fuses with the bone is crucial for implant stability. New surface treatments are being developed to enhance osseointegration and reduce immune reactions (8)
Now that you know the causes, you can choose the right materials and techniques to minimize allergic reactions and ensure long term success of dental implants.
Wer kann Zahnimplantate bekommen? Generally, anyone with good overall health and sufficient bone density can be a candidate for dental implants.
However, certain health conditions and medications can affect the success of the procedure.
| Material Typ | Biokompatibilität | Hypoallergenic Properties | Common Uses |
|---|---|---|---|
| Titan | Hoch | Low | Dental implants, surgical instruments |
| Zirkoniumdioxid | Hoch | Hoch | Dental implants, crowns, bridges |
Symptoms of Dental Implant Allergies
Recognizing the symptoms of dental implant allergies is key to timely diagnosis and management.
Common Symptoms
Allergic reactions to dental implants can manifest in many ways.
Localized Symptoms: Patients may experience redness, swelling and discomfort around the implant site. These symptoms can be mistaken for post-op responses, but if they persist (3), it may be an allergic reaction.
Oral Discomfort: Some individuals report a metallic taste or burning sensation in the mouth, which can be a sign of an allergic reaction to the implant materials (3)
Severe Reactions
In rare cases severe reactions can occur.
Systemic Reactions: Although rare, systemic reactions like hives, difficulty breathing or anaphylaxis can occur from dental implants. These need immediate medical attention (7)
Chronic Complications: Peri-implantitis, a condition where inflammation and bone loss occur around the implant, can be worsened by allergic reactions and, if not addressed, can lead to implant failure (7)
| Symptom Type | Beschreibung | Frequency of Occurrence |
|---|---|---|
| Localised Symptoms | Redness, swelling, and discomfort around the implant site | Gemeinsame |
| Oral Discomfort | Metallic taste or burning sensation in the mouth | Less Common |
| Systemic Reactions | Hives, difficulty breathing, or anaphylaxis | Seltene |
| Chronic Complications | Peri-implantitis involving inflammation and bone loss | Occasional |
Diagnosis of Dental Implant Allergies
Proper diagnosis is key to managing dental implant allergies.
Allergy Testing
Testing for allergies related to dental implants can help identify the problem before it becomes a problem.
Patch Testing: This involves applying small amounts of the suspected allergen to the skin to see if there’s a reaction. Patch testing is a common method to diagnose allergies to metals like titanium and other implant materials (4)
Blood Tests: Specific blood tests can measure the levels of antibodies produced in response to the implant materials. These tests can confirm the allergic reaction (4)

Clinical Evaluation
A thorough clinical evaluation is necessary to rule out other complications.
Symptom Assessment: Clinicians should assess symptoms like swelling, pain and redness around the implant site. If symptoms persist it may be an allergic reaction rather than post-op healing (7)
Medical History Review: Review of patient’s medical history including known allergies or previous reactions to metals can be helpful in diagnosis and treatment planning (9)
Treatment and Management
Proper treatment and management of dental implant allergies is key to long term success of the implants.
Patients with conditions like dental implants and diabetes require special attention and monitoring to ensure successful outcomes.
Immediate Interventions
Immediate interventions are needed to manage the allergic reaction and prevent further complications.
Medications for Symptom Relief: Antibiotics like amoxicillin can be used to reduce the risk of implant failure. Studies have shown that 2g or 3g of amoxicillin one hour preoperatively can reduce implant failures (4)
Temporary Removal of Implant: In severe cases temporary removal of the implant may be needed to manage the allergic reaction and prevent further complications.
Long term solutions
Long term solutions focus on preventing future allergic reactions and ensuring the stability of the implants.
Alternative Implant Materials: Using alternative materials like zirconia or ceramics can reduce the risk of allergic reactions. These materials are being researched for biocompatibility and durability (2)
Ongoing Monitoring and Care: Regular follow up appointments and proper oral hygiene practices are key to prevent complications and manage allergic
Prevention of Dental Implant Allergies
Preventing allergic reactions to dental implants is key to long term success of the implants.
Pre-implantation Testing
Pre-implantation testing can help identify the allergy before the implant procedure.
Patch Testing: Patch testing is a common method to diagnose allergies to metals like titanium. This involves applying small amounts of the suspected allergen to the skin to see if there’s a reaction (2)
Lymphocyte Transformation Test (LTT): LTT is another test that can indicate a reaction to titanium. This test measures the transformation of lymphocytes in response to the allergen (2)
Patientenaufklärung
Patient education is key to informed decision making.
Material: Patients should be informed about the materials used in dental implants and their potential to cause allergic reactions. Alternative materials like zirconia and ceramics can be used for patients with known allergies (3)
Post-op Care: Proper post-op care and follow up appointments are key to monitor for allergic reactions and long term success of the implants (10)
Schlussfolgerung und wichtige Erkenntnisse
Die wichtigsten Erkenntnisse:
Material: Choosing the right implant material like zirconia or ceramics can reduce the risk of allergic reactions (2)
Diagnostic: Pre-implantation tests like patch testing and LTT are necessary to identify allergies before the procedure (2)
Management: Immediate interventions like antibiotics like amoxicillin can reduce implant failures (5)
Langfristig: Regular monitoring and proper oral hygiene is key to prevent complications and success of dental implants.
Schlussfolgerung:
Now you know the causes, symptoms and management of dental implant allergies. Patients can make informed decisions and enjoy better oral health with minimal risk. Dental professionals can deliver better treatment outcomes by using comprehensive diagnostic and management strategies.

FAQ
Referenzen
(1) Esposito M, Ardebili Y, Worthington HV. Interventions for replacing missing teeth: different types of dental implants. Cochrane Database Syst Rev. 2014;7:CD003815.
Artikel: Interventionen zum Ersatz fehlender Zähne: verschiedene Arten von Zahnimplantaten
(2) Panchal M, Khare S, Khamkar P, Bhole KS. Dental implants: A review of types, design analysis, materials, additive manufacturing methods, and future scope. Proc CIRP. 2022;105:1-6.
(3) Guillaume B. Dental implants: A review. Morphologie. 2016;100(329):189-198.
Artikel: Zahnimplantate: Ein Überblick
(4) Esposito M, Grusovin MG, Worthington HV. Interventions for replacing missing teeth: antibiotics at dental implant placement to prevent complications. Cochrane Database Syst Rev. 2013;7:CD004152.
(5) Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1(1):11-25.
(6) Misch CE. Dental implant prosthetics. St. Louis, MO: Mosby; 2005:1-1120.
Artikel: Zahnärztliche Implantatprothetik
(7) Pjetursson BE, Thoma D, Jung R, Zwahlen M, Zembic A. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implants Res. 2012;23 Suppl 6:22-38.
(8) Buser D, Sennerby L, De Bruyn H. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol 2000. 2017;73(1):7-21.
(9) Klinge B, Meyle J. Soft-tissue integration of implants: consensus report of Working Group 2. Clin Oral Implants Res. 2006;17 Suppl 2:93-96.
Artikel: Soft-tissue integration of implants: consensus report of Working Group 2
(10) Hammerle CH, Jung RE. Bone augmentation by means of barrier membranes. Periodontol 2000. 2003;33:36-53.
Artikel: Bone augmentation by means of barrier membranes


